|
Selective Lesioning Procedures in Spinal Roots and
Spinal Cord for Treatment of Spasticity |
Spasticity is one of the
most common sequels of neurologic diseases. In most patients,
spasticity is useful in compensating for lost motor strength.
However, in a significant number of patients it may become
harmful and lead to further functional losses. When not
controllable by physical therapy and medications, excessive
spasticity can benefit from neurostimulation, intrathecal
Baclofen pharmacotherapy, botulinum toxin injections, or
selective ablative surgical procedures. Lesioning can be
performed at the level of the peripheral nerves, spinal roots,
spinal cord, or the dorsal root entry zone (DREZ). Here, only
selective procedures in the spinal roots, spinal cord, and DREZ
will be described.
 PROCEDURES
PROCEDURES
 POSTERIOR RHIZOTOMIES
POSTERIOR RHIZOTOMIES
After Sherrington demonstrated in 1898 that decerebrate rigidity
in an animal model was abolished by section of the dorsal roots
(that is, by interruption of the afferent input to the
monosynaptic stretch and polysynaptic withdrawal reflexes),
posterior rhizotomy for the modification of spasticity was first
performed by Foerster in 1908. Its undesired effects on sensory
and sphincter function have limited its application in the past.
To minimize these disadvantages, several authors in the 1960s
and 1970s attempted to develop more selective operations,
especially for the treatment of children with cerebral palsy.
 Posterior Selective Rhizotomy
Posterior Selective Rhizotomy
To reduce the sensory side-effects of the original Foerster
method, Gros and coworkers introduced a technical modification
that consisted of sparing one rootlet of the five of each root,
from L1 to S1. On similar principles, Ouaknine, a pupil of Gros,
developed a microsurgical technique that consisted of resecting
one third to two thirds of each group of rootlets of all the
posterior roots from L1 to S1.
 Sectorial Posterior Rhizotomy
Sectorial Posterior Rhizotomy
In an attempt to reduce the side-effects of rhizotomy on
postural tone in ambulatory patients, Gros and his pupils Privat
and Frerebeau proposed a topographic selection of the rootlets
to be sectioned. First, a preoperative assessment of spasticity
useful for postural tone (abdominal muscles, quadriceps, gluteus
medius) and spasticity harmful to the patient (hip flexors,
adductors, hamstrings, and triceps surae) is conducted. Mapping
of the evoked motor activity of the exposed rootlets, from L1 to
S2, by direct electrostimulation of each posterior group of
rootlets is then carried out, and the rootlets to be sectioned
are determined according to the preoperative program.
 Partial Posterior Rhizotomy
Partial Posterior Rhizotomy
Fraioli and Guidetti reported on a procedure by which the dorsal
half of each rootlet of the selected posterior roots is divided
a few millimeters before its entrance into the posterolateral
sulcus. The authors report good results without significant
sensory deficit, the latter being explained by the fact that
partial section leaves intact a large number of fibers of all
types.
 Functional Posterior Rhizotomy
Functional Posterior Rhizotomy
The search for specially organized circuits responsible for
spasticity led Fasano and associates to propose a new method
called functional posterior rhizotomy. This method is based on
bipolar intraoperative stimulation of the posterior rootlets and
analysis of different types of EMG reflex responses. Responses
characterized by a permanent tonic contraction, an
after-discharge pattern, or a large spatial diffusion to distant
muscle groups were considered to belong to disinhibited spinal
circuits responsible for spasticity. Functional posterior
rhizotomy—which was especially conceived for children with
cerebral palsy— has also been used by other outstanding surgical
teams, each one having brought its own technical modifications
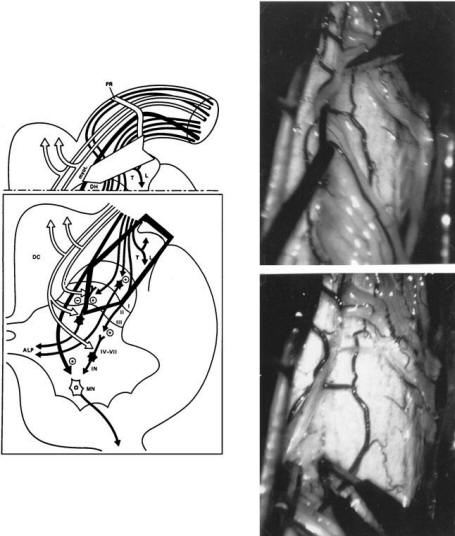
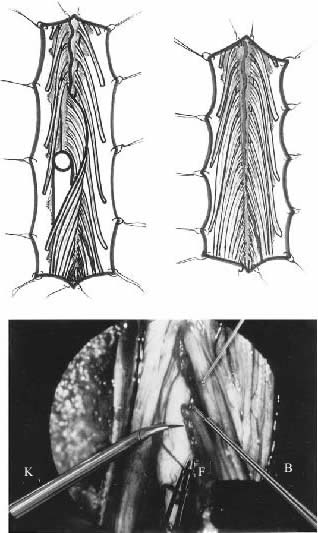
to the method. Adaptation of these methods is illustrated in
Fig.1.
 RESULTS OF POSTERIOR RHIZOTOMIES
RESULTS OF POSTERIOR RHIZOTOMIES
The results of posterior rhizotomies in children with cerebral
palsy—whatever the technical modality may be—have been recently
reported in several publications. Briefly, these publications
show that about 75% of the patients had nearly normal muscle
tone at 1 year or more after surgery without spasticity limiting
the residual voluntary movements of the limbs. After a serious
and persisting physical therapy and rehabilitation program, most
children demonstrated improved stability in sitting and/or
increased efficiency in walking. It must be noted, however, that
preexisting orthopedic deformities cannot be improved with this
method.
| |
 |
|
| |
FIGURE.1 Lumbosacral posterior rhizotomy for children with
cerebral palsy. The technique consists of performing a
limited osteoplastic
laminotomy using a power saw, in one single piece, from T11 to
L1 (left). The laminae will be replaced at the end of the
procedure and fixed with wires
(right). The dorsal (and ventral) L1, L2, and L3 roots are
identified by means of the muscular responses evoked by
electrical stimulation performed intradurally
just before entry into their dural sheaths. The dorsal sacral
rootlets are recognized at their entrance into the dorsolateral
sulcus of the conus
medullaris. The landmark between S1 and S2 medullary segments is
located approximately 30 mm from the exit of the tiny coccygeal
root from the conus.
The dorsal rootlets of S1, L5, and L4 are identified by their
evoked motor responses. The sensory roots for bladder (S2–S3)
can be identified by monitoring
vesical pressure. Those for the anal sphincter (S3–S4) can be
identified by rectomanometry (or simply using finger introduced
into the patient’s rectum)
or EMG recordings. Surface spinal cord SEP recordings from
tibial nerve (L5–S1) and pudendal nerve (S1–S3) stimulation may
also be helpful.
For the surgery to be effective, a total amount of 60% of dorsal
rootlets must be cut (with a different amount of rootlets cut
according to the level and
function of the roots involved). Also, the correspondence of the
roots with the muscles having harmful spasticity or useful
postural tone must be considered
in determining the amount of rootlets to be cut; in most cases,
L4 (which predominantly gives innervation to the quadriceps
femoris) has to be
preserved. |
|
 LONGITUDINAL MYELOTOMY
LONGITUDINAL MYELOTOMY
Longitudinal myelotomy, which was introduced by Bischof,
was made
more selective by Pourpre and later on by Laitinen.
The method consists
of a frontal separation between the posterior and anterior horns
of the
lumbosacral enlargement from T11 to S2 performed from inside the
spinal
cord after a posterior commisural incision that reaches the
ependymal canal.
In Laitinen’s series of 25 patients, 60% had complete relief of
spasticity and 36%
showed some residual spasticity in one or both legs. Within 1
year, some muscular
tone returned in most patients but seldom produced troublesome
spasticity.
A harmful effect on bladder function was present in 27% of the
patients.
Longitudinal myelotomy is indicated only for spastic paraplegias
with flexion
spasms, when the patient has no residual useful motor control
and no bladder
and sexual function.
 SURGERY IN THE DORSAL ROOT ENTRY
ZONE (DREZ)
SURGERY IN THE DORSAL ROOT ENTRY
ZONE (DREZ)
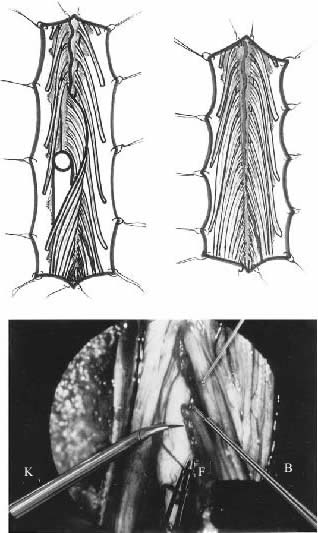
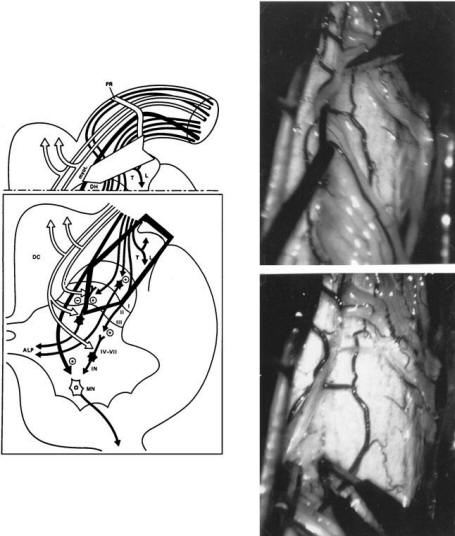
Selective posterior rhizotomy in the dorsal root entry zone
(DREZ), referred to
as micro-DREZotomy (MDT), was introduced in 1972 to treat
intractable
pain. Because of its inhibitory effects on muscular tone, it has
been applied to
patients with focalized hyperspasticity. This method
attempts to selectively
interrupt the small nociceptive and the large myotatic fibers
(situated laterally
and centrally, respectively), while sparing the large lemniscal
fibers which
are regrouped medially. It also enhances the inhibitory
mechanisms of Lissauer’s
tract and the dorsal horn (Fig.2 left).
MDT, the technique of which has been described elsewhere, consists
of microsurgical incisions that are 2 to 3 mm deep and at a 35°
angle for
the cervical level (Fig.2 right) and at a 45° angle for the
lumbosacral level
(Fig.3), followed by bipolar coagulations performed
ventrolaterally at the
entrance of the rootlets into the dorsolateral sulcus, along all
the cord segments
selected for operation. For patients with paraplegia, the
L2–S5
segments are approached through a T11-L2 laminectomy, whereas
for the
hemiplegic upper limb, a C4–C7 hemilaminectomy with
conservation of
the spinous processes is sufficient to reach the C5–T1 segments.
Identification
of the cord levels related to the undesirable spastic mechanisms
is achieved
by studying the muscle responses to bipolar electrical
stimulation of the anterior
and/or posterior roots. The motor threshold for stimulation of
anterior
roots is one third that of the threshold for posterior roots.
Then, the lateral
aspect of the DREZ is exposed so that the microsurgical
lesioning can be performed.
Lesions are 2 to 3 mm in depth and are placed at 35 to 45°
angles in the
ventrolateral aspect of the sulcus all along the selected
segments of the spinal
cord. Intraoperative neurophysiological monitoring may be of
some help for
identifying cord levels, quantifying the extent of MDT, and
avoiding impairing
long fiber tracts.
| |
 |
 |
|
| |
FIGURE.2 Micro-DREZotomy (MDT). Left, organization of fibers
at the DREZ in humans. The
large arrow shows the proposed extent of the MDT affecting the
lateral and central bundles formed
by the nociceptive and myotatic fibers, as well as the
excitatory medial part of the Lissauer Tract
and the upper layers of the dorsal horn. Right, principle behind
the MDT technique. Example of the
MDT at the cervical level through a right cervical
hemilaminectomy (the procedure for the lumbosacral
roots is the same). The right C6 posterior root has been
retracted toward the inside to make the
ventrolateral region of the DREZ accessible. The incision is
performed into the dorsolateral sulcus
using a small piece of razor blade (upper operative view). The
incision is 2 to 3 mm deep and is
made at a 35° angle (at a 45° angle for the lumbosacral level).
Then microcoagulations are created
with a very sharp and graduated bipolar microforceps down to the
apex of the dorsal horn (lower
operative view). |
FIGURE.3 MDT technique at the lumbosacral level. Top left,
exposure of the conus medullaris through a T11–L1 laminectomy.
Bottom left, approach
of the left dorsolateral sulcus. For this approach, the rootlets
of the selected lumbosacral dorsal roots are displaced dorsally
and medially to obtain proper
access to the ventrolateral aspect of the DREZ. Right, the
rootlets of the selected dorsal roots are retracted
dorsomedially. They are subsequently held with
a specially designed ball-tip microsucker, used as a small hook
to gain access to the ventrolateral part of the DREZ. After the
fine arachnoidal filaments
sticking the rootlets together with the pia mater are divided
with curved sharp microscissors (B), the main arteries running
along the dorsolateral sulcus
are dissected and preserved, while the smaller ones are
coagulated with a sharp bipolar microforceps (F). Then, a
continuous incision is performed using a
microknife (K) made with a small piece of razor blade inserted
within the striated jaws of a curved razor blade holder (K). The
cut is—on average—at
a 45° angle and to a depth of 2 mm. The surgical lesion is
completed by doing microcoagulations under direct magnified
vision, at a low intensity, inside
the posterolateral sulcomyelotomy down to the apex of the dorsal
horn. These microcoagulations are made by means of the special
sharp bipolar forceps
(F), insulated except for 5 mm at the tips and graduated every
millimeter. |
|
MDT is indicated in paraplegic patients, especially when they
are bedridden
as a result of disabling flexion spasms, and in hemiplegic
patients with irreducible
and/or painful hyperspasticity in the upper limb. MDT
also can
be used to treat neurogenic bladder with uninhibited detrusor
contractions
resulting in leakage of urine around a catheter.
To date, Sindou et. al. series has consisted of 45 patients with unilateral
cervical
(C5–T1) MDT for harmful spasticity in the upper limb, 121
patients with bilateral
lumbosacral MDT (L2–S1 or S5) for disabling spasticity in the
lower limbs,
and 12 patients with bilateral sacral S2–S3 (S4) MDT for
hyperactive neurogenic
bladder only. Effects on muscular tone can be judged only after
a 3-month
follow-up. A “useful” effect on spasticity, allowing withdrawal
of antispasmodic
medications, was obtained in 78% of the patients with a spastic
upper limb. A
similarly useful effect was obtained in 75% of the patients with
spasticity in the
lower limbs. When spasms were present in paraplegic patients,
they were suppressed
or markedly decreased in 88% of the patients. When compared to
patients with multiple sclerosis (75% with good results), the
results were better
in patients with spasticity (and spasms) caused by pure spinal
cord lesions (80%
with good results). The least improvement was observed in
patients with spasticity
resulting from cerebral lesions (60% with good results).
Reduction in
spasticity usually leads to a significant improvement in
abnormal postures and
articular limitations. This was achieved in about 90% of our
patients.
For the hemiplegic upper limb, the increase in articular
amplitude was most
remarkable for the elbow and shoulder (when not “frozen”) and
much more
limited for the wrist and fingers, especially if there was
retraction of the flexor
muscles and no residual voluntary motor activity in the
extensors. For the lower
limb(s), with abnormal postures in flexion, the increase in
amplitude of joint
movement was very much dependent on the degree of the
preoperative retractions.
When the post-MDT gains were deemed insufficient because of
persistent
joint limitations, complementary orthopedic surgery was
indicated. With
regard to the patients (n = 5) who had paraplegia with
irreducible hyperextension,
all were completely relieved. In the patients with some
voluntary movements
hidden behind spasticity, reduction in the hypertonia resulted
in an
improvement in voluntary motor activity. Fifty percent of the
patients operated
on for spasticity in the upper limb had better motor activity of
the shoulder and
arm, but only half of those with some preoperative distal motor
function
obtained additional hand prehension. Only 10% of the patients
with spasticity
in the lower limb(s) had significant motor improvement after
surgery (because
most patients in this group had no preoperative motor function).
In these
severely affected patients, the main benefit was better comfort,
less pain, ability to resume physical therapy, and less
dependence in daily life. Bladder capacity was significantly improved in 85%
of the 38 patients
who had a hyperactive neurogenic bladder with urine leakage
around the
catheter. The 32 patients who improved were those in whom the
detrusor was
not irreversibly fibrotic. Pain, when present, was in general
favorably influenced.
MDT continually produced a marked decrease in sensation.
Because most patients were in a precarious general and
neurological state,
death occurred in 5 patients (4%), resulting from respiratory
problems in 4 and
bed sores in 1. Two patients with multiple sclerosis (MS)
presented with acute
but transient increases in their preexisting neurological
symptoms during the
postoperative period. Two others had a new postoperative
clinical manifestation
of the disease. The last of the complications to be mentioned
concerns
a patient who was operated on at the cervical level and had a
persistent motor
deficit in the ipsilateral leg after surgery.
With rigorous selection of patients, MDT can be very effective
in relieving
pain and suppressing excessive spasticity. Good long-lasting
relief of excess
spasticity was achieved in 80% of our patients. As a result,
MDT, sometimes
combined with complementary orthopedic surgery, resulted in
significant
improvement in patient comfort and joint deformities, and even
enhancement
of residual voluntary motility hidden preoperatively behind
hypertonicity.
 INDICATIONS
INDICATIONS
 INDICATIONS FOR SURGERY IN ADULTS INDICATIONS FOR SURGERY IN ADULTS
 Spinal Cord Stimulation
Spinal Cord Stimulation
Provided that the spasticity is mild and the dorsal columns are
still functioning,
spinal cord stimulation can be useful for treating spasticity
from diseases affecting
the spinal cord (e.g., MS or degenerative diseases such as
Strumpell-Lorrain
syndrome). A percutaneous trial before a definitive implantation
may be useful.
 Intrathecal Baclofen Intrathecal Baclofen
Intrathecal baclofen administration is indicated for para- or
tetraplegic patients
with severe and diffuse spasticity, especially when spasticity
has a spinal origin.
Because of its reversibility, this method should be used before
an ablative procedure
is considered. But the range between excessive hypotonia with
loss of strength
and an insufficient effect is very narrow. An intrathecal test
through a temporary
access port can be useful when deciding if permanent
implantation is indicated.
| |
 |
|
| |
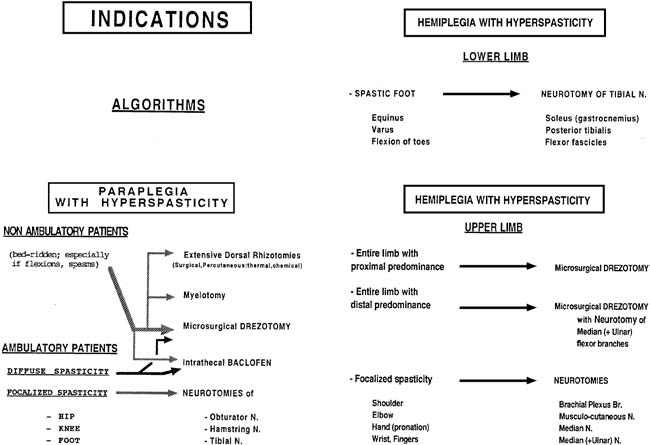
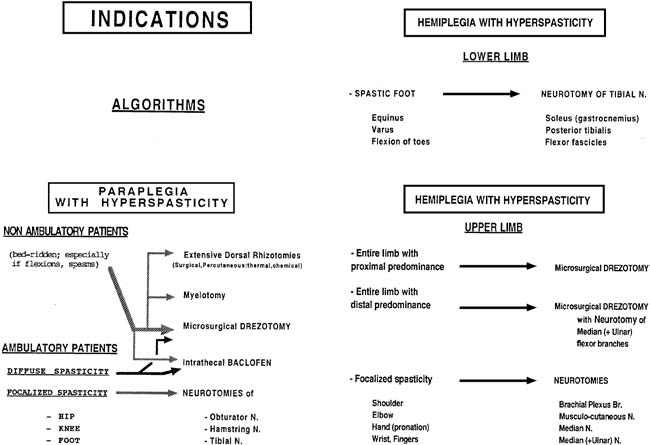
FIGURE.4 Decision-making for hyperspasticity in adults. |
|
 Neuroablative Techniques Neuroablative Techniques
Neuroablative techniques are indicated for severe focalized
spasticity in the
limbs of paraplegic, tetraplegic, or hemiplegic patients.
Neurotomies are preferred
when spasticity is localized to muscle groups innervated by a
small
number of, or a single, peripheral nerve (or nerves). When
spasticity affects an
entire limb, MDT is preferred. Several types of neuroablative
procedures can be
combined in the treatment of one patient, if needed.
Whatever the situation and the etiology may be, orthopedic
surgery should
be considered only after spasticity has been reduced by physical
and pharmacological
treatments first and, when necessary, by neurosurgical
procedures. Guidelines for surgical indications are summarized in Fig.4. The general rule is to tailor
individual treatments
as much as possible to the patient’s particular problems.
 INDICATIONS FOR SURGERY IN CHILDREN
WITH CEREBRAL PALSY INDICATIONS FOR SURGERY IN CHILDREN
WITH CEREBRAL PALSY
Surgical indications depend on preoperative abilities,
disabilities, and the eventual
functional goals. As a means of guidance, it is adopted the
six-group
classification as defined by Abbott.
 Independent Ambulatory Patients
Independent Ambulatory Patients
In independent ambulatory patients, the goal is to improve
efficiency and cosmetics
in walking by eliminating as many abnormally responsive neural
circuits as can
be identified through functional posterior rhizotomy. Surgery is
best performed as
soon as possible after the child has demonstrated the ability to
work with a therapist,
usually between ages 3 and 7 years, and frequently must be done
in conjunction
with operations on tendons because of concomitant shortened
muscles.
 Ambulatory Patients Dependent on Assistance Devices
Ambulatory Patients Dependent on Assistance Devices
For ambulatory patients dependent on assistance devices (canes,
crutches, rollators,
walkers), the goal is to lessen that dependence. A child with
poor trunk
control or lack of protective reaction but with good underlying
strength in the
antigravity muscles can safely undergo a functional posterior
rhizotomy. In
children dependent on hypertonicity in the quadriceps to bear
weight, a limited
sectorial rhizotomy is preferable. For children who are in the
process of developing
ambulatory skill and need a temporary assistance device, it is
important
to delay surgery until they have perfected these skills.
 Quadruped Crawlers
Quadruped Crawlers
For quadruped crawlers (or bunny hoppers) the goal is to achieve
assisted
ambulation during mid-childhood to early adolescence. A
functional posterior
rhizotomy will decrease hypertonicity in the leg musculature and
allow better
limb alignment in the standing position for a child with
adequate muscular
strength. However, a child who exhibits quadriceps weakness can
be considered
for a sectorial posterior rhizotomy. Children in this group can
present at a
young age with progressive hip dislocation. The goal is to stop
the progressive
orthopedic deformity by using obturator neurotomy with adductor
tenotomies
or functional posterior rhizotomy.
 Commando (or Belly) Crawlers
Commando (or Belly) Crawlers
For commando (or belly) crawlers disabled by severe deficiencies
in the postural
control, the goal of posterior rhizotomy is only to improve
functioning in
the sitting position by increasing stability.
 Totally Dependent Children
Totally Dependent Children
In totally dependent children with no locomotive abilities, the
goals are to
simply improve comfort and facilitate care. As with group 4
(commando [or
belly] crawlers), the preferred treatment is posterior
rhizotomy, but there is also
a need for exploring the efficacy of intrathecal baclofen.
 Children with Asymmetrical Spasticity
Children with Asymmetrical Spasticity
For asymmetrical spasticity, selective peripheral neurotomies
must be considered,
especially obturator and tibial for a spastic hip or foot,
respectively. For
upper limb spasticity, the MDT procedure and/or selective
neurotomies of the
flexor muscles of wrist and fingers can be considered.
 CONCLUSION
CONCLUSION
Spasticity is usually a useful substitute for deficiencies in
motor strength. Therefore,
it must be preserved. Although it happens infrequently, it can
lead to the
harmful aggravation of a motor disability. When excessive
spasticity is not sufficiently
controlled by physical therapy and pharmacological agents,
patients can
consider surgery, especially neurosurgical procedures. By
suppressing excessive
spasticity, correcting abnormal postures, and relieving the
frequently associated
pain, surgery for spasticity allows physiotherapy to be resumed
and sometimes
results in the reappearance of, or improvement in, useful
voluntary motility.
When dealing with these patients, the surgeon must know the
risks of the available
treatments. To minimize those risks, the surgeon needs a strong
anatomic,
physiological, and chemical background, rigorous methods to
assess and quantify
the disorders, and the ability to work in a multidisciplinary
team.
|


 POSTERIOR RHIZOTOMIES
POSTERIOR RHIZOTOMIES